When it comes to making advances in health informatics, taking a look at the different interoperability layers within healthcare and the standards that are used to exchange data between health systems is key.
The Healthcare Information and Management Systems Society (HIMSS) defines interoperability within 4 levels: Foundational, Semantic, Structural and Organizational
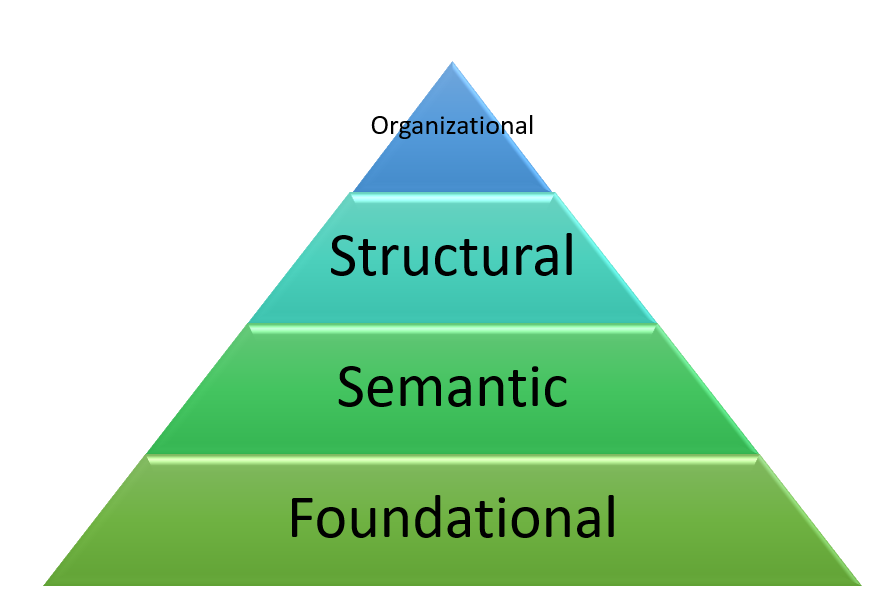
Foundational
This is the most basic form of interoperability where health information is exchanged between two or more different healthcare systems. The information just has to be passed through securely without any interpretation of the health information sent by the receiving system.
Structural
Unlike foundational interoperability, structural interoperability refers to the process of sharing data between two or more healthcare systems, where the data is interpreted at the data field level. When it comes to facilitating this sharing process you might have heard about Health Level Seven (HL7) Standard, which is an electronic messaging standard used for data exchange. For instance, Admission Discharge and Transfer messages are common messages sent which are triggered as the patient passes through the healthcare organization (e.g., if the patient is transferred to the intensive care unit). As observed through this example, the receiving healthcare system (EMR or Emergency Department) has to be able to receive and understand this trigger event (i.e. patient being transferred) and should be able to “read” and store personal health information (e.g., patient health card identifier, name, date of birth etc…) sent.
Semantic
While most organizations are working on foundation and structural interoperability, semantic interoperability is the goal. To be able to not only interpret the healthcare data being received from another healthcare system but to be able to use that data to drive and improve patient outcomes. You might have heard of standards, such as ICD-10 (International Classification of Diseases) and SNOMED-CT (Systematized Nomenclature of Medicine – Clinical Terms). These standards are used to classify and document different diseases and disorders. Whereas, SNOMED-CT is used primarily for documenting clinical terminology within the EHR and ICD-10 is used for classifying diseases and disorders. SNOMED-CT can be used for clinical analytics whereas, ICD-10 can be used for billing purposes.
When it comes to providing meaning from healthcare data being received, imagine a situation where there is a free-text document with written clinical information. To interpret this document one might use Natural Language Processing and a clinical documentation standard, such as SNOMED-CT, to extract clinical meaning from this unstructured free-text data. You can see an example below, taken from a case study from SNOMED International’s Confluence:

Organizational
The data governance framework of an organization is key as it facilitates secure and successful transfer between different organizations. This framework may include guidelines around the privacy, security and data sharing agreements, to allow this transfer to occur.
This has been a brief overview of the different layers of interoperability standards within the healthcare system. There are many other healthcare standards not discussed in this blog post that are integrated within these different layers to keep health information exchange continuous and timely.
0 Comments