You might have heard me refer to creating a clinical business intelligence portfolio to distinguish yourself from others when applying for health informatics roles. In this blog post I want to dive into how clinical business intelligence can help to improve patient outcomes and as a result, its importance within healthcare.
“If you can’t measure it, you can’t improve it.” – Peter Drucker
Clinical business intelligence can be described as a suite of tools and programs with a focus on measuring clinical metrics (e.g. patient re-admission rates, patient satisfaction scores etc…). Some of these tools might include data visualization tools such as Power BI, Tableau and Excel. There are many tools that exist and if you have an analyst’s mindset you might want to dive directly into analyzing the data but I believe that the first step should be having conversations with frontline staff on what the issues are that they see daily in their roles and how these business intelligence tools can help aid or reduce the burden on their tasks.
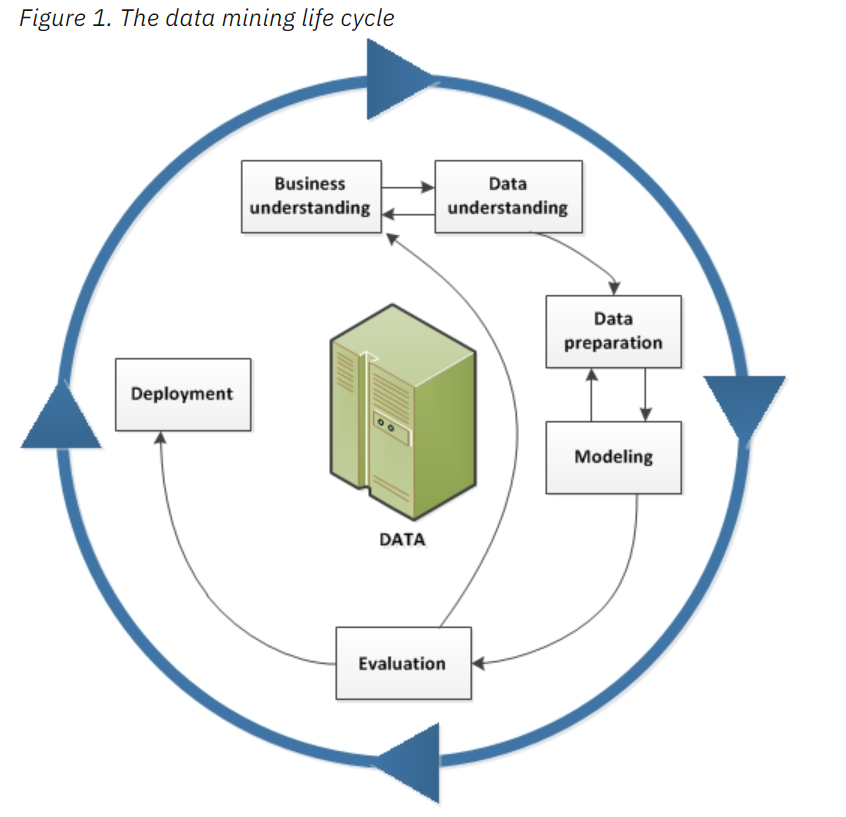
When it comes to coming up with a clinical business intelligence plan I always refer to the CRISP-DM (Cross-Industry Standard Process for Data Mining) methodology developed by IBM.
If you want to create your own clinical business intelligence portfolio you can follow along here:
In the CRISP-DM methodology, Business (Clinical) understanding is fed by Data understanding and vice versa and this is a similar situation for the clinical business intelligence plan where the clinical staff will drive an understanding of the data needed to be analyzed.
During my master’s degree, the focus of my research was to identify key clinical factors that a clinician could use to determine if there would be a risk of premature birth for the pregnant individual. What was used to shape my analysis was conversations with the clinicians on what were already risk factors that would be flagged, so I could remove them from my analysis, as it wouldn’t add any additional value to helping to optimize their workflow. This is an example of how having conversations with clinicians to understand the scope of the problem is key, prior to beginning your analysis, to ensure the results will be of value.
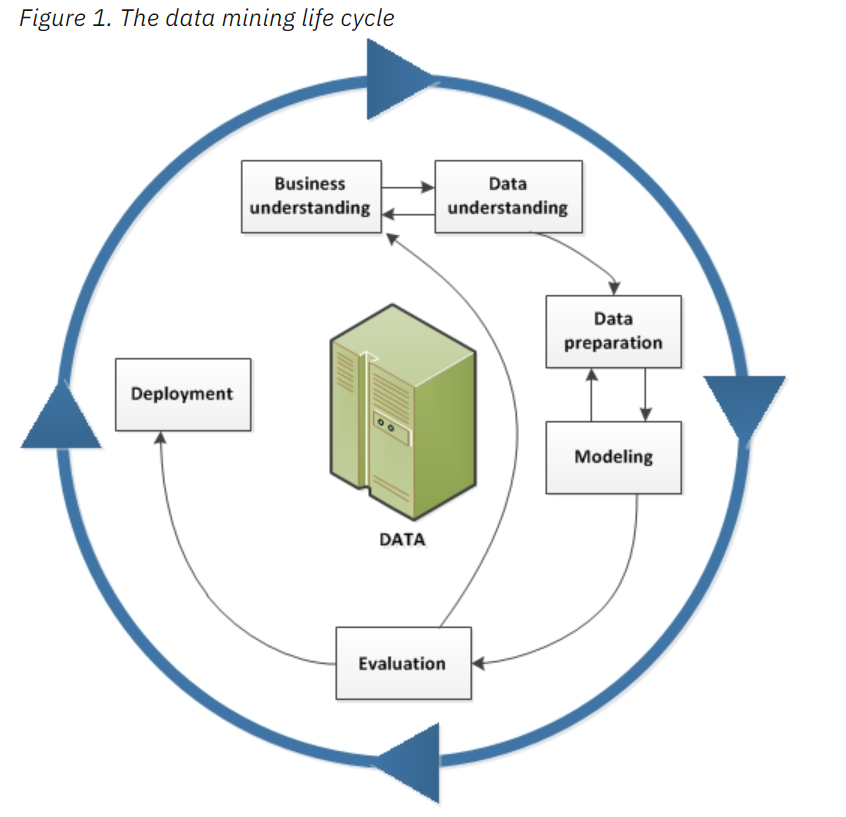
As we follow the arrows, we see that Data Preparation feeds the Modeling aspect and vice versa. This is key when using machine learning models such as Artificial Neural Networks because these models often need to have datasets without missing data.
When it comes to clinical datasets, especially survey data which might ask sensitive questions to patients who might prefer not to answer. Missing data is a common feature of clinical data. Understanding the type of modelling you will be using might influence the type of data preparation and cleaning of the data that would need to be done, to ensure the modelling portion is successful.
Data preparation is one of the areas that can take the bulk of the analyst’s time, however, there are some great tools such as Power Query, that can be found in both Excel and Power BI, which can help you to remove trailing whitespace issues, unnecessary columns and rows in your dataset, pivot your data and more. Tools such as SQL, which stands for structured query language, can also help to prepare your raw messy data into actionable information. Whether modelling is a result of creating a data visualization in the form of a report or dashboard or building a predictive model, 9 times out of 10, if you are dealing with clinical data there will need to be some form of cleaning the data.
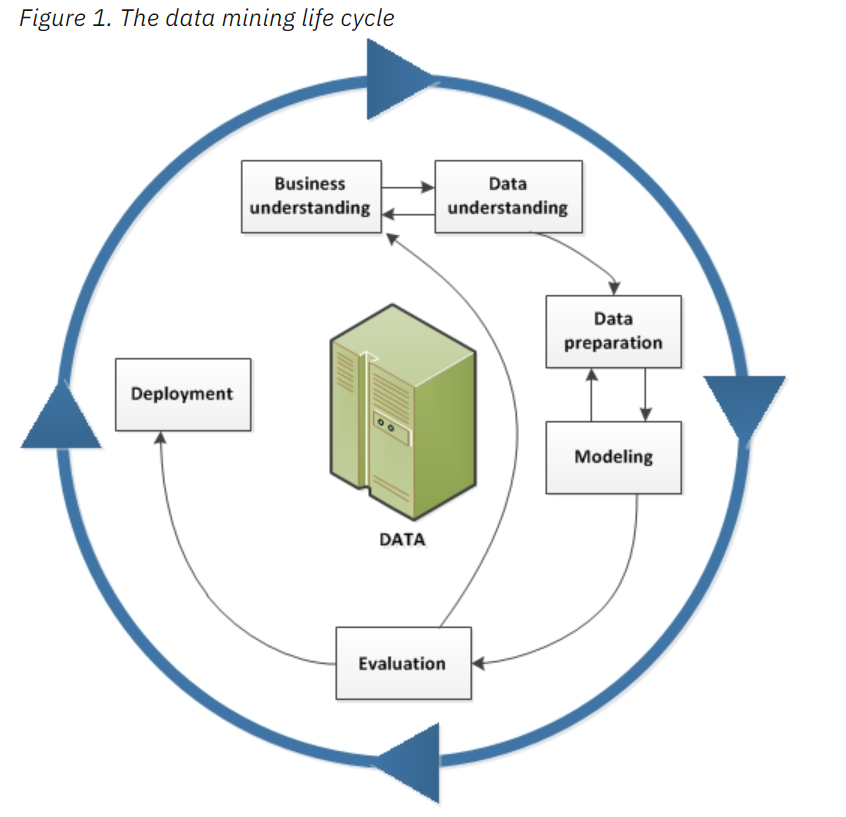
The next step is Evaluation and as you can see it feeds back into the Business understanding. In previous posts and on the Health Analytic Insights podcast, I have stated that communication skills are a key part of the health informatics role because oftentimes you will have to present your analysis to clinical stakeholders, who will be able to provide further guidance on if your analysis can be implemented immediately or needs further tweaking. More and more articles are reporting on the use of these black-box AI models implemented in a clinical setting, when few individuals actually understand the back-end of the tool. A drive for interpretable models to understand how certain predictions are being made is on the rise, especially to protect marginalized groups who are often the ones who might be harmed by these blind predictions.
The final step to this clinical business intelligence plan is Deployment of the model and integration of the tool to help improve clinical workflow and patient outcomes. Healthcare is always rapidly changing and this model is an iterative process that constantly needs to be improved and adjusted.
I hope this post has illuminated the importance of clinical business intelligence and how it can help to drive patient outcomes and improve healthcare delivery.
0 Comments