I recently listened to an interesting podcast episode of Today, Explained by Vox all about the vaccine distribution. How the vaccine will be distributed will vary widely from country to country and the rollout plan will vary widely as the year progresses. However, the primary focus across Canada will be centred on high-risk populations such as long-term healthcare workers, adults in indigenous populations and long-term care residents.
The vaccine represents a light at the end of a dark tunnel and shows the testament of scientific research and discovery as these vaccines were developed in record breaking-time. The ability for richer nations to quickly obtain large quantities of vaccines for their citizens has given me pause to be lucky to live in Canada, whereas, other nations will have difficulty obtaining the vaccine and disseminating the vaccine to their citizens. Some reports show that poorer nations might not have access to fully vaccinate their citizens until 2024. This got me thinking about the topic of health equity and how it presents in the field of health informatics.
What is health equity?
The WHO defines health equity as “The absence of unfair and avoidable or remediable differences in health among population groups defined socially, economically, demographically or geographically”
Health equity is a complex challenge to tackle within healthcare systems but if we can apply it to health informatics, can we make a difference in our day to day lives to help bridge the gaps in our healthcare systems using technology? 
Telemedicine and Health Equity
We see an example of this due to the widespread adoption of telemedicine during the pandemic, I had several virtual doctor’s visits throughout 2020 and I noticed significant time savings. For those who don’t have access to cars or who cannot take time off work for extended periods, telemedicine could be a solution to skipping the waiting room. Also, access to telemedicine can be a great benefit for those who live in rural areas or remote areas with limited access to clinical staff.
However, telemedicine is not the be and end-all, some people do not have secure access to phones, desktops and laptops. Also, some groups do not have the technological literacy to access these applications effectively. Care should be made when designing these clinical portals to access telemedicine to ensure the user-interface is as straightforward as possible. Telemedicine is not the solution to all care, as older populations can have difficulty hearing or seeing the doctor through a screen. When in-person visits resume having the option to have virtual appointments for low-risk populations might free up the doctor’s time to focus on high-risk groups and populations.
As 5G technology develops and we move towards a more technologically connected world, currently libraries offer digital literacy programs, and as it seems telemedicine is here to stay, developing these programs to keep up with the changing times will be important to help reduce educational barriers to healthcare.
Disruptive Technologies and Health Equity
In the past few years, there has been a push by Uber and Lyft to disrupt the healthcare industry by providing ride-sharing services to patients by connecting directly to electronic health record platforms such as Cerner. The purpose is to allow caregivers to schedule free or affordable rides for patients who don’t have access to transportation to travel to and from medical appointments. The purpose is also to reduce the number of missed appointments which could increase existing health conditions. Similarly, Lyft has partnered with EHR vendor Allscripts.
However, early research has shown that the integration of these ride-sharing companies has not made a significant decrease in the number of no show appointments. Dr. Krisda lead study author stated “We were surprised that the effect was no difference between groups,” “We think this is likely because we didn’t have a high percentage of people who agreed to use the service or ultimately used it after agreeing,” “We think this may be the result of the way we delivered the service or lack of familiarity.”
Another criticism of the study came from Lisa Sharp, a researcher at the University of Illinois, she stated that the study didn’t assess patients’ previous experiences with ridesharing services or their perceptions about it, and it’s possible they were worried about drivers refusing to come to minority or low-income neighbourhoods.
Having a strong understanding of the health equity barriers that people are facing is critical when it comes to rolling out the latest technology. Although we have the systems in place it’s important to ensure that they will be used. This is a common thread I see working in the data analytics and business intelligence space. This notion that “if we build it, they will come“. Instead, it’s important to have a good sense of what people want to see even before building your tool to ensure it will have a lasting impact.
AI Algorithms and Health Equity
When it comes to building algorithms that are used in the healthcare field the data that is fed into the model must be analyzed, understood and biases are uncovered before developing programs that can have real-world implications on marginalized groups.
A paper published in Science identified a widely used healthcare algorithm that increasingly identified white patients over black patients concerning patients who need follow-up care, even if the black patients were just as sick as the white patients. This is because the algorithm focused on cost over health inequities that black and minority populations face.
Black populations across America generally tend to have lower incomes than white populations and because the algorithm was focused on costs and people who have lower incomes are less likely to have insurance or they might be more likely to miss appointments, due to the issues I discussed previously, this results in overall smaller health-care costs. Because the algorithm was focused primarily on costs, the algorithm identified only 18% of black patients versus 82% of white patients for follow-up care, however, when you focus on how sick someone is the number jumps from 18% to 46% when it comes to referring black patients for follow-up care.
This issue in the algorithm was only uncovered when doctors themselves took the time to delve into the data and decode the algorithm, it’s estimated this algorithm was used to suggest follow-up care for 70 million patients. Racial biases when building algorithms are widely documented and can continue to negatively affect our healthcare populations if we are not careful to understand the parameters and the data we are feeding into algorithms and ensuring we are not bringing in our own biases and lack of understanding of the populations being served.
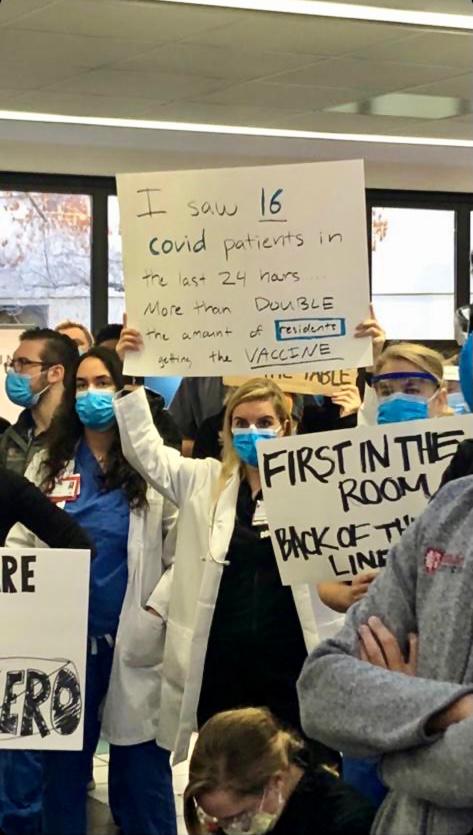
More recently, Standford Medicine was caught in hot water when it’s algorithm prioritized administration and staff who work from home to receive the COVID-19 vaccination over front-line healthcare workers. Initially, their response was to blame the algorithm but we need to move away from this thinking that AI is some external robot that is going to take over the world and understand that it is simply a mathematical tool that requires human understanding, analysis and empathy to make better decisions.
The algorithm in question was rule-based and might have looked at factors such as age, job title and general health risks for COVID-19. Depending on the weight attributed to these factors, if there was a higher weight attributed to age, then administrative staff and more established doctors who are working from home might be picked up by the algorithm versus younger residents who are working in the hospital on a day to day basis.
One lesson that can come out from all of this is the importance of constant iteration and tuning of these healthcare models. This is critical, instead of blindly relying on the output of the algorithm and deploying it without taking a step back and questioning will this model affect minority populations negatively and have I uncovered all potential biases in my data?
P.S. My book suggestion for learning more about the use of machine learning and health equity is Automating Inequality by Virginia Eubanks
Whether it comes to analyzing healthcare data, designing algorithms or building healthcare systems it’s always important to have the principles of health equity at the back of your mind. The healthcare system is rapidly evolving and with major players such as Amazon and Google disrupting the field we should be cognizant of the systems we are designing and how they will affect patients.
I would love to hear from you, how does health equity make its way into your job in health informatics? Comment down below 😃
2 Comments
The Ultimate Guide to Designing a Clinical or Healthcare Dashboard - HealthAnalyticInsights · January 31, 2021 at 6:21 pm
[…] tools for end-users, understanding your audience should be the first step. In a previous blog post, I discussed how popular ride-sharing apps such as Uber and Lyft have been trying to disrupt the […]
Chatbots in Healthcare Explained - HealthAnalyticInsights · May 3, 2021 at 10:49 am
[…] is that they can help to reduce patient no-shows, I talked about the risk for patients in this blog post and how this can lead to increased adverse effects for patients who consistently miss appointments. […]